Complete with new dashboards reporting functionality business intelligence tools and improved security FileHandler Enterprise is the new benchmark for Claims Management Software. Medicare Part D Medicaid.
 Pbm Basics Pharmacists Society Of The State Of New York
Pbm Basics Pharmacists Society Of The State Of New York
Automated Prior Authorization PA systems.

Pbm claims adjudication software. A pharmacy benefits manager is an organization or system that provides administrative and pharmacy claim adjudication services and pharmacy benefit coverage programs. E-Prescribing and ProDUR programs. The core of PBM Express is the adjudication program.
This model is very similar to how retail pharmacy is set up. Hospice Long Term Care Programs. ClaimPays PSAO is a highly respected Pharmacy Services Administration Organization PSAO.
Our clients vary from single and multi provider clinics to billing services with hundreds of providers. This flexibility delivers custom program configurations that reduce setup and on-going maintenance. The Tredium System is a PBM claims processing platform that is fully customizable and brandable to meet the needs of any customer.
LakerSoftware is actively monitoring the Coronavirus COVID-19 pandemic and taking all necessary precautions to ensure your continued access to safe medications. AClaim has been a leader in the development of online point-of-service pharmacy healthcare technology for over 20 years. One of the design principles used is the concept of time travel This principle enables the platform at an administrative level to show the configuration of the plan in a moment in history.
Lakers advanced software solution provides clients with superior. PDMI offers transparent pass-through pharmacy claims processing and pharmacy benefit administration services for private label Pharmacy Benefit Managers PBMs vertically integrated health plans and hospital systems. Designed for hospitals and healthcare centers it is a cloud-based soution that automates processes including billing scheduling payment processing reporting claims scrubbing and more.
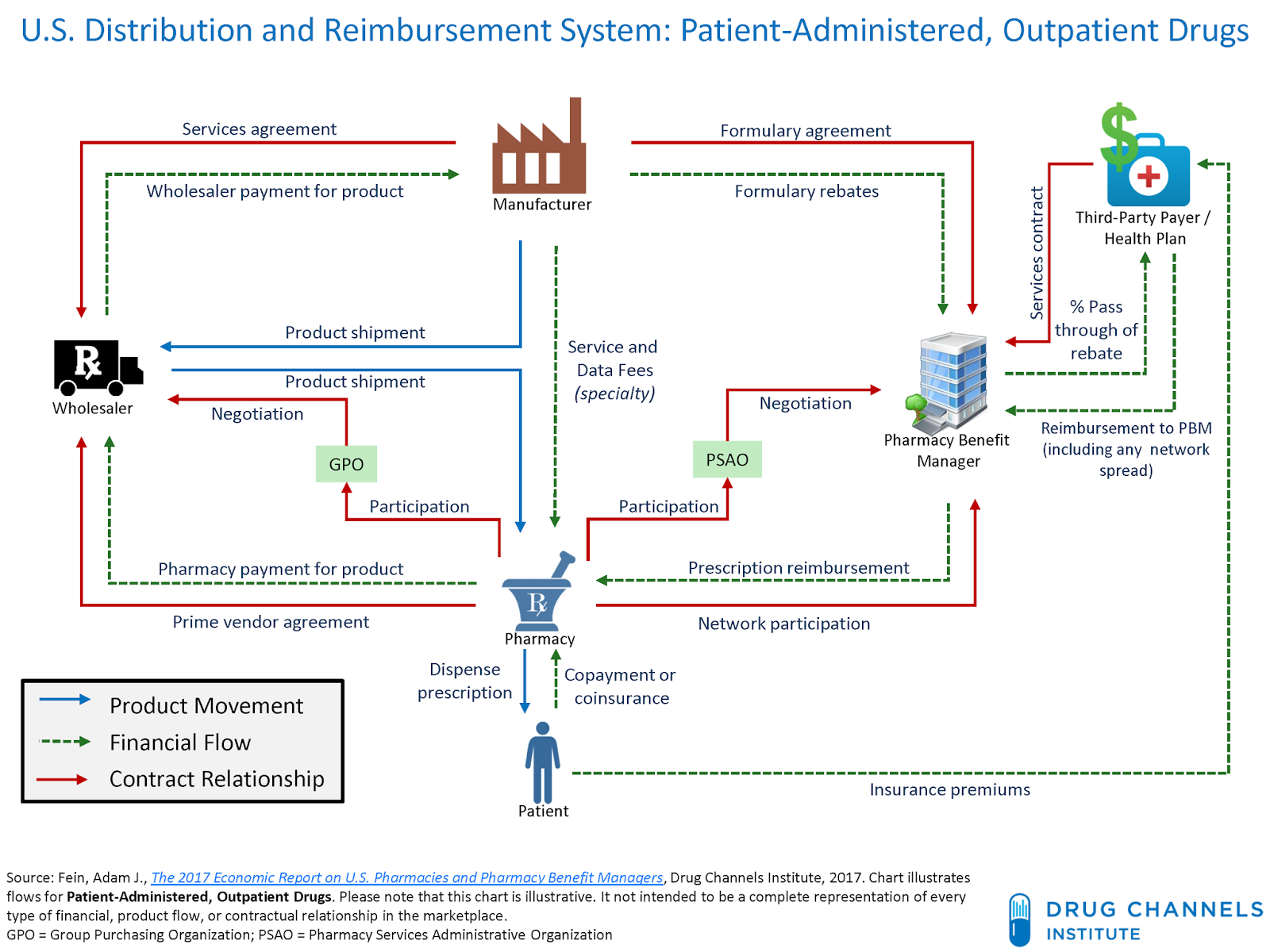
Predominantly electronically transmitted claims online and in real time Also paper claims PBMs also contract with pharmacies for dispensing services and pharmaceutical manufacturers for medications Pharmacy Benefit Manager Pharmacy Insurer Manufacturer. Experience the flexibility of addressing various. Ohri is responsible for business development product management RD and marketing.
PLEXIS comprehensive enterprise platform is the premier claims adjudication and benefit administration software solution on the market. At Tredium Solutions we used the latest technologies to build a fast highly flexible and fully customizable PBM claims adjudication platform. Serving a large number and variety of healthcare payers for the past 20 years PLEXIS simplifies and automates claims processing operations.
Our PBM solutions scale to serve the needs of state government healthcare and other programs. Claims undergo hundreds of edits to achieve accurate processing results regardless of the difficulty of the plan design. As an independent software solutions company Laker Software provides Claims Processing Systems and support services for prescription drug benefit programs.
The parameter drive program provides for an extremely flexible architechture that allows for client customization as needed. Increase process efficiency and standardization by empowering your users to perform manual tasks digitally and reduce human intervention. This model involves insurance claims adjudication patient prescription copayments and third party reconciliation of claims.
Insurance Claims Management Software. Core activity to all PBMs is pharmacy claims adjudication processing. Adjudicate Pharmacy Claims Manage Benefits.
Adjudicate pharmacy claims swiftly. Our platform is designed to manage claims and transactions in real time within seconds. Tredium offers competitive network services ranging from broad-based networks to select and custom networks.
Rebate Other Services. Automate the entire claims journey from omnichannel intimation of the first notice of loss to fraud detection and claims adjudication and finally claims settlement. Contracting with a network of pharmacies Establishing payment levels for provider pharmacies Negotiating rebate arrangements.
We currently deliver cost-efficient results to 28 programs in 21 states and the District of Columbia. Built from scratch the heart of RxSenses PBM platform is an asynchronous rules-based engine the core of claims adjudication. Contain prescription costs for your plan by accessing our wide variety of services and support to keep you on the leading edge of pharmacy administration.
PLEXIS agile flexible technology is eminently configurable to empower you to manage all aspects of claims. Datascans pharmacy software includes the ability to process claims to any PBMplan your practice is. For example rule changes can be created and assigned at various levels.
RelayHealths ProPBM software platform leverages rules-driven pharmacy designs to deliver innovative solutions that give benefit analysts needed options for design control. PBM Express Adjudication Software. AClaim builds automated real-time processing without the restraints common in many claims.
Our clients are empowered to choose the services provided by PDMI and which services kept in house. Shawns experience spans multiple domains in the PBM industry including claims adjudication pharmacy contractingnetworks softwareproduct development digital. What is a PBM.
ClaimPays PSAO Pharmacy Services Administration Organization provides effective solutions to assist pharmacy and physician owners in managing the business administration and financial components related to commercial pharmacy claim adjudication. FileHandler Enterprise is an intuitive claims administration system designed to help streamline and automate workflows for the claims and risk management market. We will process your claim in speeds unmatched in the industry.
PBM services can include.